News & Insights
News & Insights
BOOK: JOE PUBLIC 2030
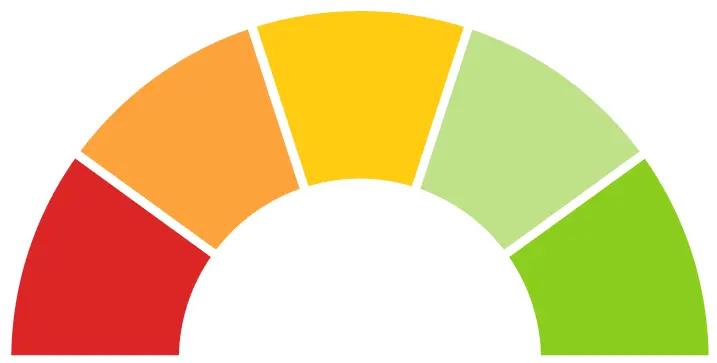
Predict-O-Meter
Joe Public 2030 makes five bold predictions about the future, which range from exciting and promising to ominous and discouraging. Through the Predict-O-Meter, we’ll continuously assess the state of the healthcare industry to track the accuracy of the five predictions.